����ժ Ҫ����Ŀ��:̽���Գ�Ѫ����MRI���ź��ݱ���̼��ص�,����Գ�Ѫ��MRI���ˮƽ������:�ռ��ٴ�ȷ����Գ�Ѫ����18����MRIӰ������,���ݳ�Ѫʱ���Ϊ�������ڡ������ڡ��Ǽ������ڡ��Ǽ��Ժ��ں�������,���л��߾�����MRI����T1WI��T2WI��T2flair(Flair)��DWI����ɨ��,��������Ѫ���ź��ص㡣���:18��������,��������3��,Ѫ��MRI����ΪT1WIΪ�Ե��ź�,T2WIΪ�Ȼ��Ը��ź�,FlairΪ�Ը��ź�,DWIΪ���ź�,��Χ�����ˮ��;������4��,Ѫ�ױ���ΪT1WIΪ���ź�,T2WIΪ���ź�,FlairΪ���ź�,DWIΪ�����ź�,��Χ���ˮ��;�Ǽ�������4��,Ѫ�ױ���ΪT1WI��T2WI��Flair��DWIΪ����ڵ��ź�,��Χ�ض�ˮ��;�Ǽ��Ժ���3��,Ѫ�ױ���ΪT1WI��T2WI��Flair��DWIΪ���ź�,��Χ���ˮ��;������4��,Ѫ��MRI�ϱ���ΪT1WI��T2WI��Flair��Ϊ���ź�,DWIΪ���ź�,��Χ��ˮ�ס�����:�Գ�Ѫ��Ѫ�ijɷ�����ʱ����ƽ����仯,���²�ͬ��Ѫ��MRI�źŴ���������,��������ɿ������ٴ���ϡ�
�����ؼ��ʣ����Գ�Ѫ; �Ź������; �ݱ����; ���;
�����Գ�Ѫ���Ƴ����ļ�֢,������Ѫѹ���Գ�Ѫ[1]�������ˡ����������Ѻ��������е�,���г�Ѫ�������з����ʽ�����ȱѪ�Ժ�˨����������,��һ�ָ��²������ļ���[2]������CT�����ýϵ͡�����졢�Լ������Գ�Ѫ�����ȷ,һֱ���Գ�Ѫ����ѡ����ֶ�[3],��MRI���Թ�������ѡ��鷽���������ҹ�����ˮƽ��MRI��鼼�������,MRIԽ��Խ���Ӧ���������е���ѡ�����,����Ѹ���ж���������,�������������ƴ�[4]������, ���ع�����Ժȷ����Գ�Ѫ18����������,������ͬʱ���Գ�Ѫ����MRI�ź��ص㡣
����1�� �����뷽��
����1.1�� һ������
����2016��1����2019��2���ڰ���ʡ®��������ҽԺ������Գ�Ѫ����18��,��11��,Ů7��;����44��73��,ƽ��(56.2±11.7)��;���г�������(<24h)3��,������(1��3d)����4��,�Ǽ�������(3��7d)4��,�Ǽ��Ժ���(8��30d)3��,������(>1��)4��;��Ѫ��λ�ֲ�:��������Ѫ6��,�Ұ��ʽ�������Ѫ3��,��Ҷ��Ѫ��5��,ӲĤ�³�Ѫ4��;�ٴ�֢״��ͷʹ������֫��������Ż�µȡ�
����1.2�� ��鷽��
�������л��߾�����MRIƽɨ��顣ʹ�������� Avanto1.5TMRI(Siemens,�¹�),ɨ���������:���ÿ��������ز�TSE���н���ˮƽλT1WI��T2WI��T2flair(Flair)����ɢ��Ȩ����(DWI)ɨ��,����T1WI(TR/TE200ms/4ms)��T2WI��Flair(TR/TE 7500ms/90ms),ɨ����Ϊ5mm,����2mm��DWIʹ�õ��μ�������-ƽ��ز�����SE-EPI,TR/TE:4200ms/102ms,����192×192,���5mm,��ɢ��������bȡ1000s/mm2����2λӰ���ҽʦ������Ϻ�MRI�ź�������

����2 �����
����18���Գ�Ѫ���߸��ݲ���ʱ���Ϊ�������ڡ������ڡ��Ǽ������ڡ��Ǽ��Ժ��ں������ڡ�����,�������ڻ���Ѫ��MRI����ΪT1WIΪ�Ե��ź�,T2WIΪ�Ȼ��Ը��ź�,FlairΪ�Ը��ź�,DWIΪ���ź�,��Χ�����ˮ��(��ͼ1);������Ѫ�ױ���ΪT1WIΪ���ź�,T2WIΪ���ź�,FlairΪ���ź�,DWIΪ�����ź�,��Χ���ˮ��(��ͼ2);�Ǽ�������ʱѪ�ױ���ΪT1WI��T2WI��Flair��DWIΪ����ڵ��ź�,��Χ���ض�ˮ��(��ͼ3);�Ǽ��Ժ���ʱѪ�ױ���ΪT1WI��T2WI��Flair��DWIΪ���ź�,��Χ���ˮ��(��ͼ4);������Ѫ��MRI�ϱ���ΪT1WI��T2WI��Flair��Ϊ���ź�,DWIΪ���ź�,��Χ��ˮ��(��ͼ5)���������1��
������1 ��ͬѪ����MRI�ź��ص�

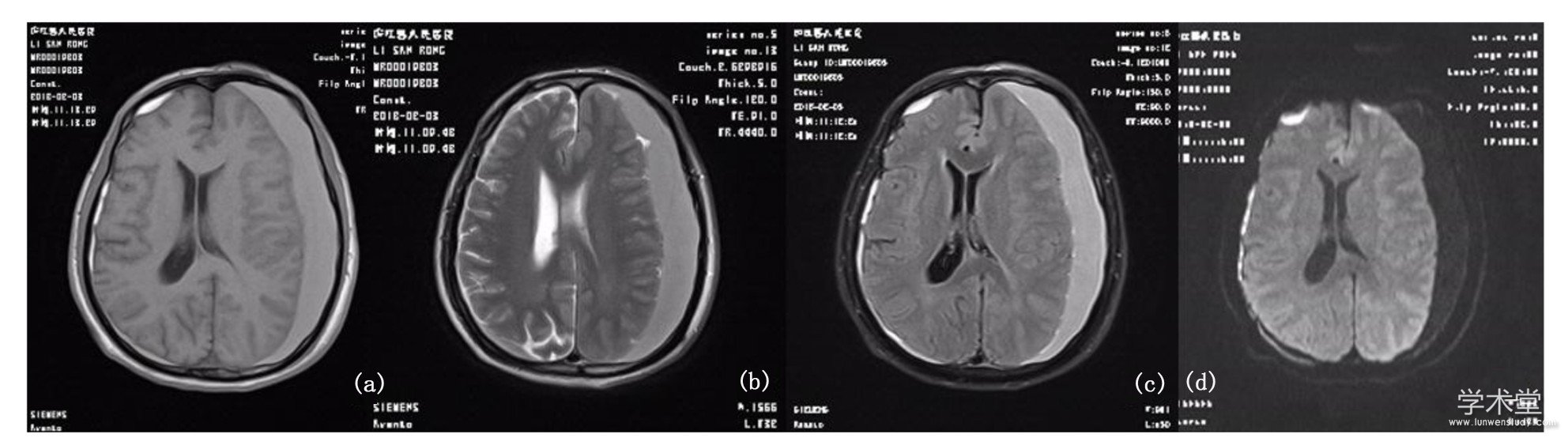
����ͼ1 �Գ�Ѫ��������Ѫ��MRI����
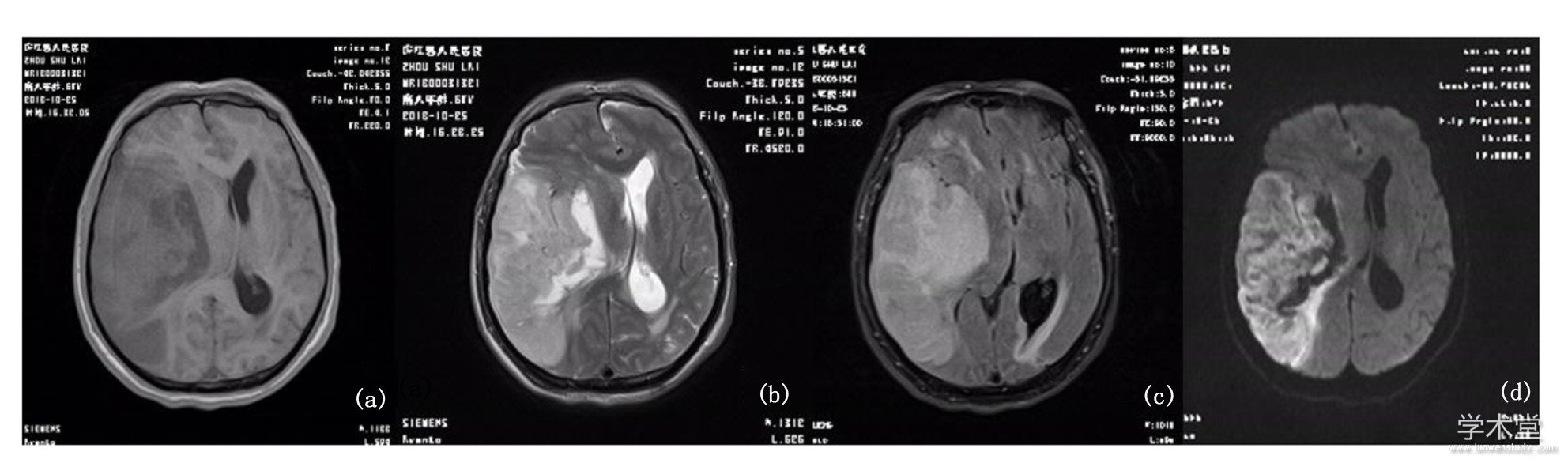
����ע:(a)T1WI�Ե��ź�;(b)T2WI�Ȼ��Ը��ź�;(c)Flair�Ը��ź�;(d)DWI���źš�
����ͼ2 �Գ�Ѫ������Ѫ��MRI����
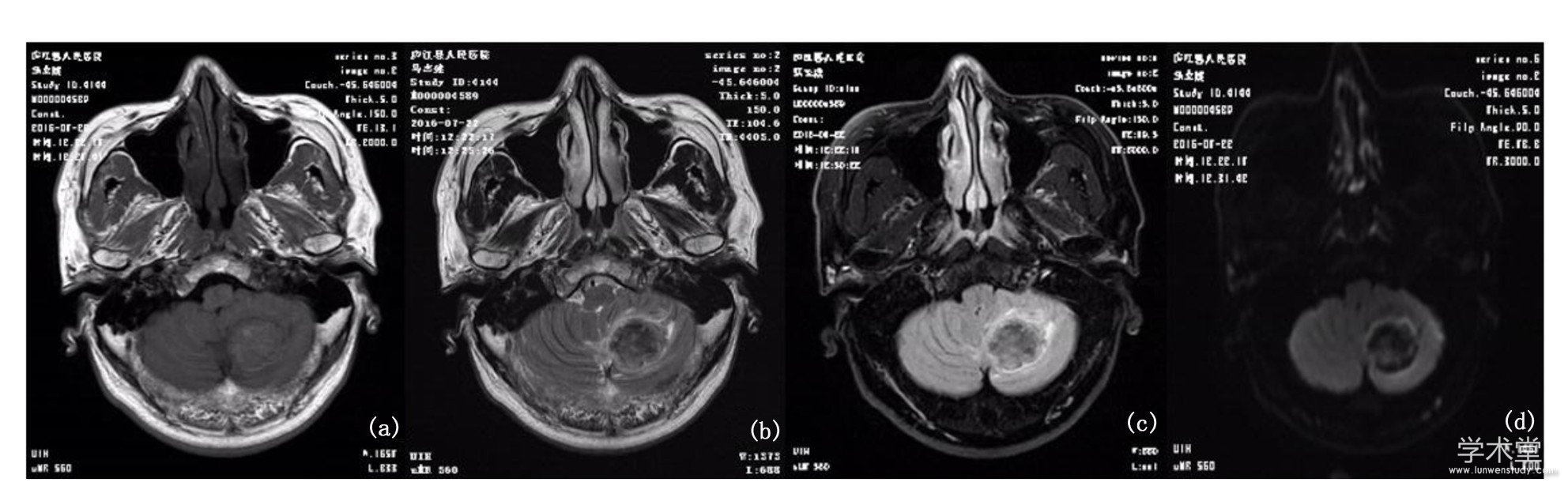
����ע:(a)T1WI���ź�;(b)T2WI���ź�;(c)Flair���ź�;(d)DWI�����źš�
����ͼ3 �Գ�Ѫ�Ǽ�������Ѫ��MRI����
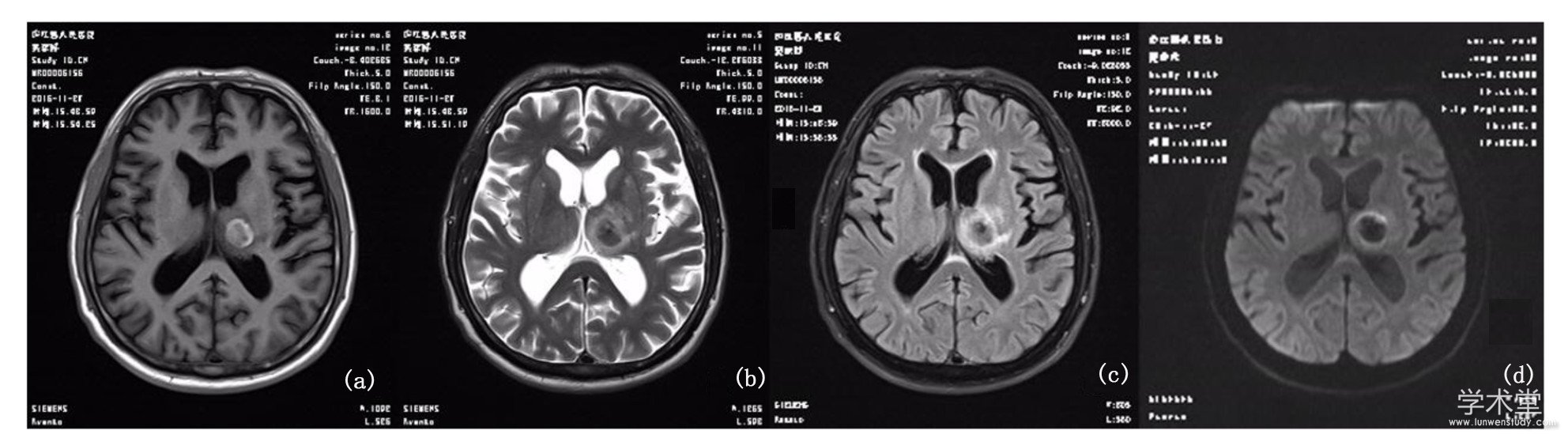
����ע:(a)T1WI����ڵ��ź�;(b)T2WI����ڵ��ź�;(c)Flair����ڵ��ź�;(d)DWI����ڵ��źš�
����ͼ4 �Գ�Ѫ�Ǽ��Ժ���Ѫ��MRI����
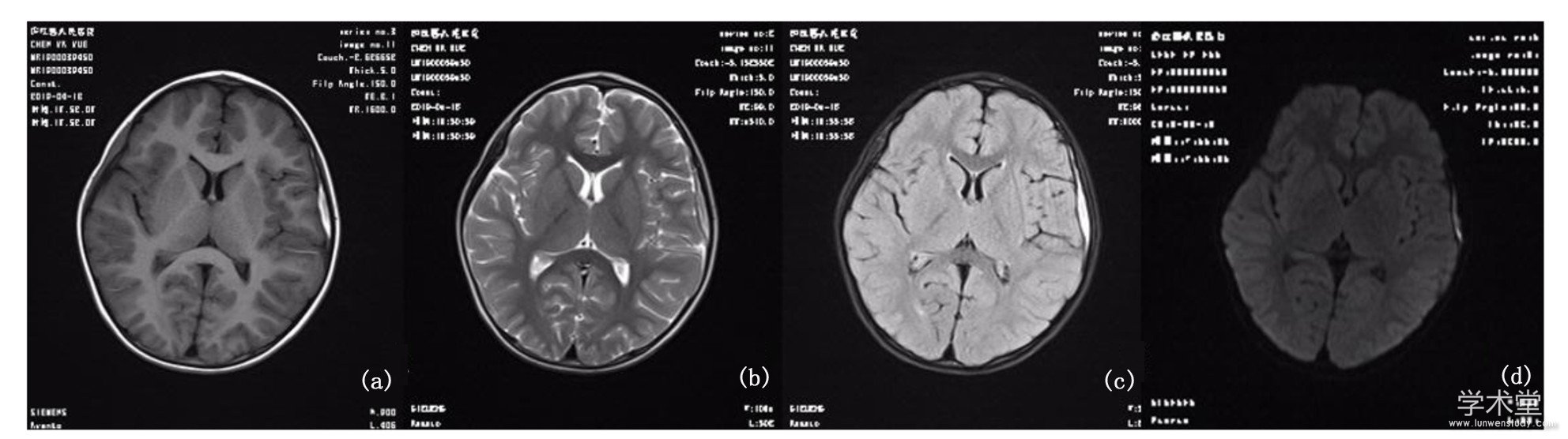
����ע:(a)T1WI���ź�;(b)T2WI���ź�;(c)Flair���ź�;(d)DWI���źš�
����ͼ5 �Գ�Ѫ������Ѫ��MRI����
����ע:(a)T1WI���ź�;(b)T2WI���ź�;(c)Flair���ź�;(d)DWI���źš�
����3�� ����
�����Գ�Ѫ���ٴ���������,�����ڶ���ԭ����ѪҺ����ʵ�ʻ�ǻ϶�ڻ���,���»���ͷʹ��Ż�¡���ʶ�ϰ���̱����,�����չѸ��Σ��,�²������ʸߡ�����ȷ�������,�������Ž���������,�����Ԥ��[5]�������Գ�Ѫ��Ҫ����ͷ��CT����ȷ��,���г���Ѹ�١����ýϵ͵�����,�������ٴ�֢״���Ƶ����Թ������������е�����ʲ���[6],�������ҹ�ҽ��ˮƽ�����,MRI������ռ�,����ٴ�֢״���Ƽ���������ʸ���,����������Flair��DWI���ڸ����Գ�Ѫ����Ϻͼ�����ϼ�ֵ��,�������ٴ����ߡ�
�����ٴ��϶����Գ�Ѫ���ڲ�δͳһ,ͨ������ѪС��24h����Ϊ��������,1��3dΪ������,4��7dΪ�Ǽ�������,8��30dΪ�Ǽ��Ժ���,����1��Ϊ������[7]����Ѫ�׳�ʼ�ɷ�ΪѪҺ,�Ժ�ϸ��Ϊ��,�ں�����Ѫ�쵰��,����ʱ����ƽ�,������ɷ��仯,���������ӵķֲ��ʹŻ�״̬�ı�,��Ҳ�Dz�ͬʱ��Ѫ����MRI�ź�������ͬ�Ļ���������Ѫ�쵰���ڵ������ӳʿ�����,����Ѫ�쵰�����˳����[8]����ϸ��Ĥ����ʱ�����ӷ�ɢ,�ų�Ƿ���ȵ���MRI����,����ϸ��Ĥ�����,�Ż�ЧӦ��ʧ[9]��
�����о���,��������3��,MRI�����ʾ:T1WIΪ�Ե��ź�,T2WIΪ�Ȼ��Ը��ź�,FlairΪ�Ը��ź�,DWIΪ���ź�,��Χ�����ˮ�ס���������ԭ������:��ʱѪ����δ��ȫ����,�ɷ���δ���Ա仯,�Ժ�ϸ��Ϊ��,Ѫ�쵰����ҪΪ����Ѫ�쵰��,���ж�����,ȱ�ٲ��ɶԵ���,�ʿ�����,���Գ���MRI�ϳ��ֵȻ��Ե͡��Ը��ź�,�����Ӱ��©�������;��Flair�ϳ��Ը��ź�,DWI�����ʱˮ������ɢ��δ����,���ֵ��ź�,��T1WI��T2WI���Ͽ�����ȷ���Ϊ�Գ�Ѫ��������[10]��������4��,MRI�����ʾ:T1WIΪ���ź�, T2WI��FlairΪ���ź�,DWIΪ�����ź�,��Χ���ˮ�ס���������ԭ������:����ʱ����ƽ�,Ѫ������������Ѫ�쵰������,����Ѫ�쵰��������,����ߺ���������,��4�����ɶԵ���,����˳����,���Ž���T2WI��Flair��DWI�ź�;������Ѫ�쵰�ײ����������ӵ���ż����ǿ,�ʲ�������T1WI;�����ʱ��ϸ��������ˮ,���γɸ�Ũ������Ѫ�쵰��,����Ѫ���ܱ����ˮ����[11]���Ǽ�������4��,Ѫ��MRI�ź�ΪT1WI��T2WI��Flair��DWIΪ����ڵ��ź�,��Χ���ض�ˮ�ס���������:��Ѫ�����Ǽ�������(4��7d),Hb��һ������������Hb,����5�����ɶԵ���,˳���Խ�һ����ǿ,��������T1WI,����Hb�������⼰��,�ʶ�����Ϊ��������ڵ��ź�,����Ѫ���ܱߵ����ض�ˮ��[12]���Ǽ��Ժ���3��,MRI�����ʾ:T1WI��T2WI��Flair��DWIΪ���ź�,��Χ���ˮ�ס�����ԭ������:�Ǽ��Ժ���(8��30d)Ѫ���ں�ϸ����ȫ����,Ѫ����������ʱҲ������HbΪ��,Flair��DWI�Ͼ���ʾ���ź�,�����������ϸ����ʼ����Hb�γɺ���Ѫ����,����˳����ǿ,�ʶ�T1WI��T2WIΪ���ź�,��ʱѪ���ܱ�ˮ��������[13]��������4��,Ѫ��MRI��T1WIΪ�Ը��ź�,T2WIΪ���ź�,FlairΪ���ź�,DWIΪ���ź�,��Χ��ˮ�ס�����ԭ������:������Ѫ���Ѿ�Һ��,����Hb���ȷֲ�,����ʱ������,Ѫ�׳ɷ���Ϊ�͵���Һ��,���ųɷֵĸı�,T1WI���ָߵ����ź�,T2WI��FlairΪ���ź�,DWIΪ���ź�[14]��
������֮,�Գ�Ѫ��Ѫ����������ݱ���һ�������Ĺ���,Ѫ��MRI�ź�Ҳ��֮�ı䡣����MRI�������,����ٴ����Գ�Ѫ��MRI�����,���õ��ṩ�ٴ����ƾ��ߡ�
���������
����[1]��̻�,������,�����,��.¤�����Գ�Ѫ���в�ѧ�������ٴ��ص����[J].ҽѧ������ʵ��,2019,32(5):753��755.
����[2] Sennf?lt S,Norrving B,Petersson J,et al.Long-Term Survival and Function After Stroke[J].Stroke,2019,50:53��61.
����[3] Yun B J,Borczuk P,Zachrison K S,et al.Utilization of head CT during injury visits to United States emergency departments:2012—2015[J].Am J Emerg Med,2018,36(8):1463��1466.
����[4] Bai Q K,Zhao Z G,Lu L J,et al.Treating ischaemic stroke with intravenous tPA beyond 4.5 hours under the guidance of a MRI DWI/T2WI mismatch was safe and effective[J].Stroke Vasc Neurol,2019,4(1):8��13.
����[5] Gregson B A,Mitchell P,Mendelow A D.Surgical Decision Making in Brain Hemorrhage[J].Stroke,2019,50:1108��1115.
����[6] �����,�����,������,��.CT��MRI���Թ�����������е�Ӧ��Ч���Ƚ�[J].�й�CT��MRI��־,2018,16(5):8��10,14.
����[7] Allkemper T,Tombach B,Schwindt W,et al.Acute and subacute intracerebral hemorrhages:comparison of MR imaging at 1.5 and 3.0 Tinitial experience[J].Radiology,2004,232(3):874��881.
����[8] Mohamed M,Heasly D C,Yagmurlu B,et al.Fluid-attenuated inversion recovery MR imaging and subarachnoid hemorrhage:not a panacea[J].AJNR Am J Neuroradiol,2004,25(4):545��550.
����[9] Fazeel M,Siddiqui,Simon V,et al.Neuroimaging of Hemorrhageand Vascular Defects[J].Neurotherapeutics,2011,8(1):28��38.
����[10] ������,½��.�����Գ�Ѫ�ĵͳ�MRI����[J].ʵ�÷���ѧ��־,2010,26(1):14��16.
����[11]Nighoghossian N,Hermier,Madeleine P.Old microbleeds are a potential risk factor for cerebral bleeding after ischemicstroke:a gradient-echo T2weighted brain MRI study[J].Stroke,2002,33(3):735��742.
����[12]����ƽ,�ſ�,�����,��.��ͬ�ڱ��Գ�ѪMRI��ϼ��źű仯�ص�[J].����������־,2016,24(6):376��381.
����[13]������.��ͬʱ���Գ�Ѫ�ĴŹ�����ɢ��Ȩ�����ź��ص㼰���Ӧ��[J].�й�ʵ��������־,2016,19(15):29��31.
����[14]�Ż���,����,����Ȼ,��.DWI���Գ�Ѫ����ϼ��������[J].ʵ�÷���ѧ��־,2014,30(9):15��18.
�����Գ�Ѫ���߲������Ծ��Ͱ�����̹������Ч
�����Գ�Ѫ����ˮ�ij��ּȻ���ɼ�������֯���˵ķ���, ���п��ܵ��¼̷�������֯���˵ķ������ڱ����о���Ӧ������ҩ�鷽�Ƽ����������Ծ�ע��Һ, ���Զ�Ѫ��ͨ����һ������������, ��һ���̶��ϸ��ƴ���ȱ��״̬����ϸ���Ĵ�л, ��������ˮ�Ļ���, ...
��Ѫѹ�Գ�Ѫ������ѹ���������ڿƳ�����Σ����֢������ȫ����Ч�ؼ����ѹ��������ˮ�ͽ�����ѹ������Ч�ĸ��Ʋ��鼰Ԥ���ڿƴ�ͳ��ѹ�����ȡ�����������������Լ�����Ϊ�д��Բ������������ظ�ѹ(��ѹ����350mmH2O)ʱ����...
���������������66����������Ѫѹ���Գ�Ѫ
��Ѫѹ�Ի������Գ�Ѫ������Ƴ���...
�Ի�ˮ���ڶ�����������Ĥ��ǻ��Ѫ���һ�ֽ�Ϊ����IJ���֢���ٴ��������������ͣ�����ɲ�����֪����ȱʧ���������𣬶Բ���Ԥ��������Ӱ�졣Ϊ����Ч�����Գ�Ѫ���Ի�ˮ�ķ����ʣ������о��Ա�Ժ2012��ȫ���ڿ����β�ȷ��Ϊ�Գ�Ѫ���������ҵ�50����...
PCASL�Ͷ�̬�����м�Ȩ�������Թ����е�Ӧ��
��������һ���²��ʡ������ʽϸߵij���������������ȱѪ�������з����ʽϸ�[1].��Ѫ����ע������DWI��ϣ��������ٴ�ҽʦ�˽��Թ���������������Χ��֯����Ѫ������ѧ��Ϣ��Ϊ�Թ����������ṩ������Ϣ��Ŀǰ�����õ���Ѫ����ע����������ڵ���������ˡ�...
�Գ�Ѫ��ҽѧ�繫�ϵ��²��ʸߡ������صļ�֢�����������Ե������仯���Ը��������ء���Χ�㣬��ʶ����ʧ���������ضȻ���״̬�����й����ױ������Գ�Ѫ�ķ������Ѿ����ֳ�������������ƣ���ˣ�̽�ַ��������Ч�����Գ�Ѫ���м��ߵ�ҽѧ��ֵ�����ε���...
�����ɷַ�������VBM������̽��MS-SSCI�Ӿ���
�������������Ͷ��Ӳ�����ߣ�multiplescle-rosispatientswithsimplespinalcordinvolvement,MS-SSCI����ָ�����ڳ���Ӱ���Ͻ��м��財��������ڿ��Ӳ����һ����Ӳ����multiplesclerosis,MS�����о�[1]������MS�������������о��ɷ�������ή...
��Ĥ���ķ����������ˡ��Ŵ�������������й�,���߶���������ϰ�������ϰ���֢״�����ֻ�������ѹ������ֶ��ġ�Ż�µ�֢״������о�ָ��,�ٴ�����ȷ���������Ĥ���Ը���Ԥ���л������塣...
�����������������Գ�Ѫ��Ѫ����Ч����
�ٴ�ҽѧ��,�Գ�Ѫ��Ѫ����һ��Σ����֢,�������������ô�ͳ�ı������Ʒ�����������,�����²��ʽϸ�,ͬʱ������Ӧ�������սϴ�,���ֻ����������ڼ���������������ҹ�ҽ�Ƽ���ˮƽ�IJ������,����������Ӧ��Խ��Խ�㷺���Գ�Ѫ��Ѫ���ߵ�...
ǻ϶���Թ������߲��ôŹ����������Ч��
ǻ϶���Թ�����lacunar infarction,LI����ָ��������Ը�����֧С����Ѫ�ܱڲ��䣬���¹�ǻ����������С��Χ������֯�������γɵ�ֱ��Ϊ0.5��20mm��С��ǻ��֢״һ�����Ϊͷʹ��֫����ľ�ȡ�...